

Changes in outcomes and response rates (≥3 points change in PSQI score) were also reported. Cohen d effect size, P value, and standardized mean difference (SMD) were used to measure differences in treatment outcomes. Effectiveness on comorbid somnolence, anxiety, depression, and somatic symptoms were used as secondary outcomes.
Main Outcomes and Measures The Pittsburgh Sleep Quality Index (PSQI) score and its essential subitems were used as the primary outcomes. Inverse probability of treatment weighting (IPTW) using propensity scores was applied to enable homogeneous comparisons between the 3 groups.Įxposures Treatment with dCBT-I, medication therapy, or combination therapy according to prescriptions. Three therapeutic modes (ie, dCBT-I, medication, and their combination) were compared at month 1, month 3, and month 6 (primary). Objective To evaluate the clinical effectiveness, engagement, durability, and adaptability of dCBT-I.ĭesign, Setting, and Participants This retrospective cohort study was conducted using longitudinal data collected via a mobile app named Good Sleep 365 between November 14, 2018, and February 28, 2022. Importance Although digital cognitive behavioral therapy for insomnia (dCBT-I) has been studied in many randomized clinical trials and is recommended as a first-line treatment option, few studies have systematically examined its effectiveness, engagement, durability, and adaptability in clinical settings.

Shared Decision Making and Communication.Scientific Discovery and the Future of Medicine.Health Care Economics, Insurance, Payment.Clinical Implications of Basic Neuroscience.Challenges in Clinical Electrocardiography.Subgroup Analysis Comparing the Effectiveness of dCBT-I and Combination Therapy Subgroup Analysis Comparing the Effectiveness of Medication Therapy and Combination TherapyĮFigure 8. Patient Engagement in Each of the 5 dCBT-I SessionsĮFigure 7.
COGNITIVE BEHAVIORAL THERAPY FOR INSOMNIA REVIEWS SERIES
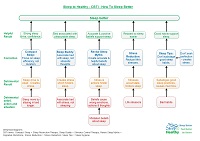
Line Charts of Time Series of the Primary and Secondary Outcomes During a 6-Month Follow-upĮFigure 6. Forest Plots of Primary and Secondary Outcomes for dCBT-I vs Combination TherapyĮFigure 5. Forest Plots of Primary and Secondary Outcomes for Medication Therapy vs Combination TherapyĮFigure 4. Interface of Good Sleep 365 AppĮFigure 3. Patient Engagement in Each dCBT-I SessionĮFigure 2. Time Series of Primary and Secondary OutcomesĮTable 9. Comparison of Primary and Secondary Outcomes in the dCBT-I and Combination GroupsĮTable 8. Comparison of Primary and Secondary Outcomes in the Medication and Combination GroupsĮTable 7. Comparison of Primary and Secondary Outcomes in the dCBT-I and Medication GroupsĮTable 6. Primary and Secondary Outcomes According to Treatment GroupĮTable 5. Improvement of Primary and Secondary Outcomes According to Treatment GroupĮTable 4. Response Rates According to Treatment GroupĮTable 3. Details of Covariates Before/After Adjustment by IPTWĮTable 2. Results of Response Rates and Changes in OutcomesĮAppendix 4. Exposure, Covariates, and OutcomesĮAppendix 3.

Current medication indicates whether the patient was taking any form of hypnotic medications at baseline.ĮAppendix 1. Medication history indicates whether the patient had a history of taking any form of hypnotic medications prior to baseline. First onset indicates whether this insomnia was the first attack. Insomnia duration refers to the length of interval from the first occurrence of insomnia to baseline. Patients with primary, middle, and senior education were classified as having low education, while patients with higher education were classified as having high education. Education level and insomnia duration were coarsely categorized to avoid overclassification resulting in a smaller sample to influence confounders’ control with inverse probability of treatment weighting. The vertical line is a reference line, placed at the value where there is no difference between 2 interventions. The last row indicates the comparison of effectiveness on the whole population. Each horizontal line represents the 95% CI of comparison (Cohen d effect size) of the Pittsburgh Sleep Quality Index score at month 6 in a subgroup, and the result is plotted as a box in the middle of the horizontal line.


 0 kommentar(er)
0 kommentar(er)
